3rd Annual Ava’s Heart Heroes Ball
Ava's Heart Heroes Ball
"Ava's Heart is the only non-profit organization in the United States that provides extensive support for transplant patients and their families, both pre and post lifesaving organ transplant. Ava's Heart founder, Ava Kaufman, is a heart transplant recipient herself."
Our transplant family and AVA KAUFMAN, Founder of Ava's Heart Heroes Ball
Ava's Heart Heroes Ball is a non-profit organization that supports transplant families with expenses incurred during hospitalizations including transportation, places to sleep and freshen up. Often times, families travel long distances to specialty hospitals (far and few between) that provide the proper care. Unfortunately, family members do not have a place to stay over the weeks-months their loved ones are hospitalized. Learning about this non-profit has been a heart warming discovery and I hope every transplant family can become aware of the services.
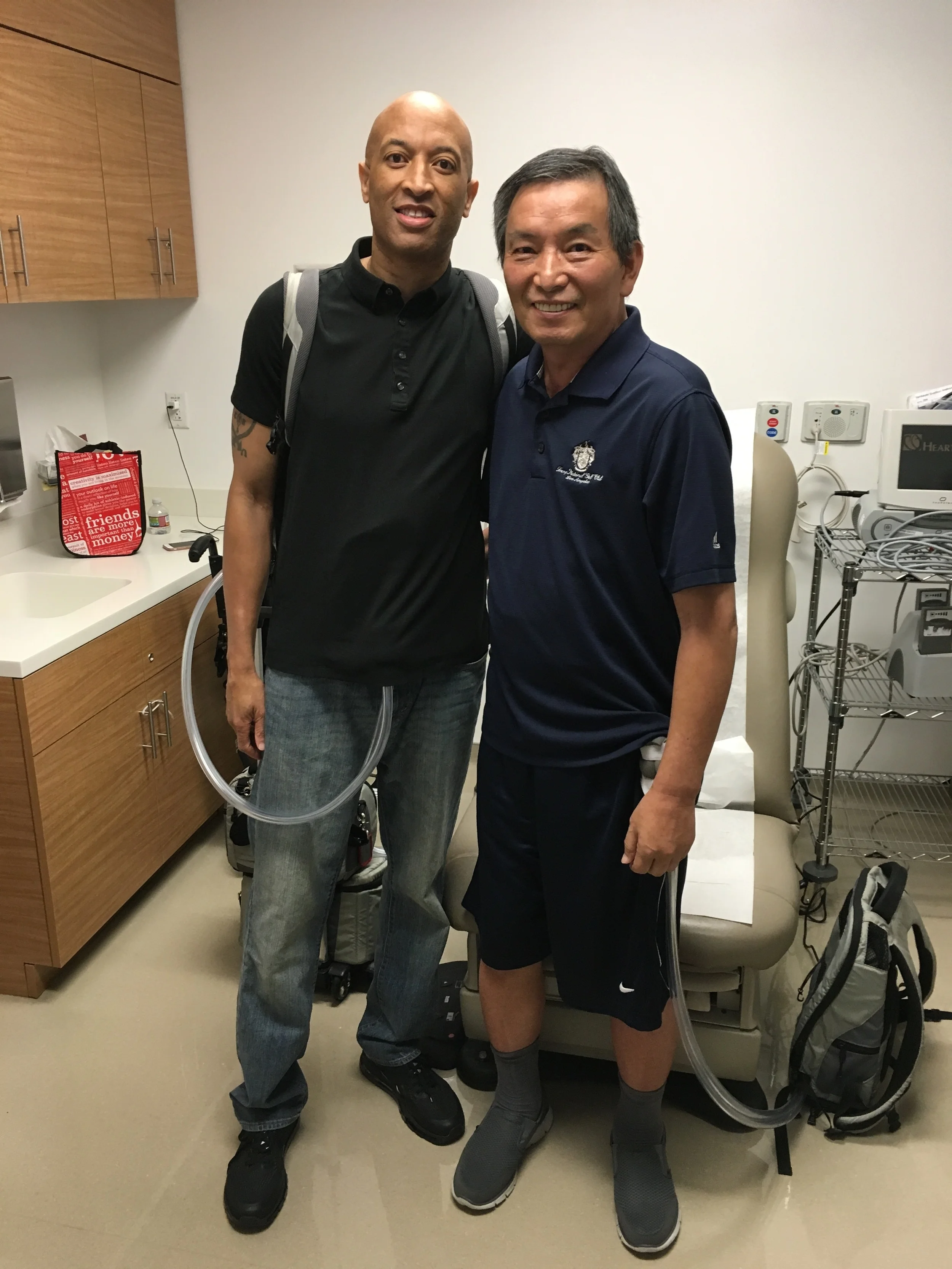
STEVE WILLIAMS, TAH & heart transplant patient, with Syncardia CEO, MICHAEL GARIPPA
Syncardia's CEO, Michael Garippa, was honored a heroes award by Ava Kaufman at her Heart Heroes Ball this past Thursday in Hollywood, CA. Our family was invited to join Syncardia's table. Unfortunately, my father has been suffering from mobility issues so only my sister Jeanne and I attended the event. We were granted additional invites so of course we extended the invites to our transplant family and their spouses. One of our favorite ICU nurses from Cedars Sinai also attended the event. It was great seeing everyone, catching up and talking about on going struggles post transplant. I was sad my dad could not attend the event; hopefully next year since the CEO of Syncardia invited us to join him again.
Everyone asked how our father was doing and I was honest about his immobility due to weakness in the legs. Another patient shared his struggling to walk post transplant, saying he was "constantly falling on my face". He told us he was able to gain strength back once he got back on an anti-rejection medication, Prednisone. His symptoms were very similar to my dad's current issues so we've since put Dad back on the anti-rejection meds to see if he gains strength. Every one is unique and our bodies respond in different ways. We can only hope he will get better from here. (Note: In August, I took 4 weeks off to help my family and take Dad to his appointments, chiropractor therapy, acupuncture and mainly to assist with physical therapy at home. I considered myself a drill sergeant and he was my soldier. After weeks of blood, sweat and tears, the results were very minimal and he got worse after the 4th week. I knew something else had to be contributing to his weakness. Stay tuned for updates.)
With our transplant family (JEANNE, me, LANCE WHITE, JOHNNY LEMUCCI, CAROLINE LEMUCCI)
With Cedars Sinai ICU Nurse, KATHY ARABIA
As a retired entertainment reporter for E! Entertainment, Us Weekly Magazine, and OK! Magazine, I've had my fair share of invitations to extravagant Hollywood parties and non-profit events. However, Ava's Heart Heroes Ball was THE MOST memorable and touching event I have ever attended. We got to hear stories from transplant patients, family members of donors, doctors, and honorees who have all been touched by transplant. Memorable monologues by Melora Hardin, Cady Zuckerman, and Joely Fisher and performances by Renee Lamontagne, Dani Hagan, Kerry King, Art Santora, Peter Michael Escoveda, Jacob Jonas The Company and Maria Howell + Tommy Coster. There's nothing like coming together to celebrate the gift of life thanks to all the donors and donor families in our community. Thank you Ava for all you do for the transplant & donor community.
LANCE WHITE, TAH & heart transplant patient, gets interviewed by KARLA GORDY BRISTOL, CEO of Bristol Entertainment.
One Year Later... Cedars Sinai's Patient Picnic
All smiles with Me, Dad and Dr. Lee
Today was Cedars Sinai's Annual Heart & Lung Transplant Patient Picnic.
Last month on June 25, 2017, marked one year since my father's heart transplant yet he is almost 95% immobile due to a combination of neuropathy, muscle & spine function/strength, and medication.
We knew Dad's inability to walk would be a challenge for today's event at the park, but showing up was important for our family to be present and celebrate how far everyone on this journey has come.
As we pushed Dad up the dirt and grass hill on his wheelchair, the gradual incline made it harder to maneuver. Two other family members saw our struggle and kindly offered their help. Thanks to their support, we got to the top where everyone had gathered.
We were reunited with other TAH (Total Artificial Heart) patients we had met at Cedars Sinai including Steve Williams, Johnny Lemucci and Lance White (all whom are back in the work force, living their best lives).
Steve Williams said getting back to work has been a new training process in itself; he needed to recondition his mind and body to get up for work everyday after years of transplant recovery.
Surrounding ourselves with our transplant families was uplifting and reminiscent of the obstacles we had all overcome. It was a reminder to be thankful we got to this point and no longer need to spend our lives at the hospital.
Dad still has a long journey ahead but our family will continue to support him and do our best to get him to recovery.
As the Cedars Sinai staff and patients hurried off to the fields to play a friendly game of baseball, our family stayed behind due to Dad's immobility. We finished up lunch, connected with a few friends and staff members then called it a day.
As we got into the car, I said to Dad, "Lets work hard this year so you can participate next year'.
Our family reunited with Steve Williams (back), a former TAH patient, our Angel on Earth, currently back in the work force
Dad with Cedars Sinai staff members Dr. Kobashigawa (left), Dr. Lee (right) and Steve Williams, fellow TAH patient (back)
Reunited with TAH patients Steve Williams (left) and Lace White (right)
Dr. Kobashigawa of Cedars Sinai welcome the patients and families
Meet Johnny Lemucchi
Earlier this year, during the hardest time of our lives in the ICU, we met the Lemucchi’s, a beautiful Italian family from Downey, CA. Unfortunately, they were in the same boat as us. A young father, Johnny Lemucchi, 55, was in desperate need of a heart but an organ was not available fast enough. Johnny received a Total Artificial Heart one day after my dad.
After spending so much time in the ICU waiting room together and learning of our loved one's fates, we bonded over updates in efforts to support, see how our fathers were healing and fighting to live.
For a month, we would spend full days in the ICU waiting room together. The grandparents patiently knitted and read the paper, the young kids would visit after school or work, Johnny’s sister and brother-in-law were always present and Caroline, Johnny’s wife would sleep over every single night in the freezing waiting room, just in case something happened.
Going through the Total Artificial Heart journey together and supporting one another has created a lasting bond between our families. We are each other’s #1 cheerleaders.
On August 20th, the same day the Lemucchi’s answered the interview questions below, Johnny received the CALL. A matching heart was available. He has since received a successful heart transplant and is currently recovering at Cedars-Sinai. We wish him a speedy recovery.
1. How did you end up with a TAH? What were your symptoms?
Caroline Lemucchi (Johnny’s Wife): He is a soccer referee and on Labor Day weekend 2015, after refereeing many games over 3 days, he felt very dehydrated and weak but still continued to work, coach soccer and referee games. After about a month of not feeling well, I made an appointment for him to get a physical. On November 6th 2015, he was given an EGG (Electrogastrogram) test and the doctor ran in and said, “You are having a heart attack!”
The paramedics rushed him to Whittier Presbyterian Intercommunity Hospital (PIH), where he was diagnosed with CHF (Congestive Heart Failure). He was told his first heart attack was sometime in September 2015 and that he needed a defibrillator installed at Cedars-Sinai.
After going into going into cardiac arrest in December 2015, Cedars Sinai inserted the device. Johnny was sent home and celebrated the holidays with family. He was feeling better then he had in months, and especially grateful to spend time with his new granddaughter. Suddenly, five weeks later, with no sign and not even feeling it, his defibrillator went off.
Cedars Sinai instructed us to take him to the nearest hospital. Feeling great after a few days in the hospital, Johnny went into cardiac arrest the night before he was scheduled for discharge.
Johnny was put on a breathing machine and placed into critical care. I was told nothing could be done his heart was badly damaged. I told them that I wanted him transferred to Cedars-Sinai, and with the help of Dr. Beckham from Whittier PIH, it was done. He was transferred the next day and after a series of tests, Johnny was on the heart transplant list. We were listed 1A Status for 3 days but no heart was available. Our last chance at life was the Total Artificial Heart.
2. What was the hardest part of your time in the hospital? What was the best part of being in the hospital?
Johnny Lemucchi: The hardest part of being in the hospital was being away from family and home. The best of being in hospital was I knew that I was in good hands, and have a lot of trust in the doctors and nurses at Cedars-Sinai.
3. During your stay at the hospital, what did your family/staff do that made a difference in making you feel more comfortable?
JL: Having my family with me and supporting me made it easier. The staff treated me with respect but during the recovery process my family’s support helped me get stronger and easier for my recovery.
CL: For me, the staff kept me informed on everything that was going on and tried to make my stay easier.
4. What do you wish your family did to help make your experience better?
JL: Just having support of family and friends made it easier on both of us.
5. Do you have any tricks that will help someone new to the TAH?
JL: Try to continue doing what you enjoy doing and don't give up on life. You might have to make a few adjustments, but make those adjustments and then go on with life. Don't let your machine keep you indoors or tied down. If people ask questions, be proud and tell them about your success with the machine.
6. Do you remember your time in the ICU? How long were you there for?
JL: I don't remember much about the ICU. I was in there for about two weeks, but I know everyone was very helpful to my family and me.
7. What is your outlook on having a TAH until a donor organ becomes available?
JL: My outlook on having TAH until I get donor heart is that I am here, being able to enjoy life and family.
8. What do you look forward to this year?
JL: I was able to attend my youngest son’s graduation from high school, middle son’s graduation from college and watch my granddaughter grow up. I am looking forward to her first birthday in October and spending the holidays with family.
9. What are your top three tips for people on the TAH journey?
JL: Take care of your TAH equipment, take your medications and make sure you change your dressing every day.
10. Any additional advice or tips for your fellow TAH friend? Last words?
JL: Don't let it keep u down. Live life to its fullest. Keep a positive attitude. That donor heart will come. Once I get my heart would like to thank donor family and meet them if possible. Once I get my heart, I want to coach and referee, travel and spend time with family.
See Johnny’s local story from The Downey Patriot here.
Meet Lance E. White
“I am currently in the hospital awaiting a heart transplant. I stay steadfast and strong, waiting to start my new life and to spread the word about the new technological advances to help heart patients.”
Lance Edward White, 49, has been a Total Artificial Heart (TAH) patient for twenty-six months and counting after being diagnosed with Congestive Heart Failure (CHF) in 2014.
Earlier this year in January, my family and I were freaking out about the unfamiliar TAH. We had just learned about the device a few hours before my dad's emergency scheduled surgery. To provide aide, our Mechanical Circulatory Support (MCS) coordinator shared Lance's contact information, offering an option to speak with someone living with the mechanical device. That night, Lance kindly took our phone call and made time to speak with my family and other families listening in on speaker phone in the freezing ICU waiting room. He assured us that life with a TAH can allow a 'new normal' life. Lance's encouraging and positive perspective gave us a true sense of relief. Hearing someone alive and well, living with the TAH was exactly what we needed in order to get through the shocking and traumatizing reality.
Fast forward a few months, on May 3, we coincidentally met Lance during a standard check-up appointment. It was exciting to meet him in person, the voice of reason who helped us overcome the mental obstacle of the Total Artificial Heart. We gave each other hugs and high fives. My family left clinic as Lance started his appointment. "See you next time," we said.
That same day, Lance was admitted to the hospital and placed on the list as Status 1A, the most urgent and highest priority. Reason being, the plastic tubes (cannulae) coming out of his abdomen had hardened after being in use for so long (over two years). Risking further cracks in the tubes would require open artificial-heart surgery with a risky TAH replacement or none at all.
Two months into his hospitalization, on June 18th, Lance got the call. Finally! Lance would get his much deserved heart transplant! He was prepped for surgery, intubated and put under anesthesia. Hours later, he woke up in the ICU... but without a new heart. While in the operating room, his surgeon and team made a difficult decision, not to proceed with the transplant. Lance stands over 6' tall which requires a larger heart for someone his size, and this particular organ was not big enough. Although initially disappointed, Lance is glad his surgeon and team made the decision they made. Choosing life is better than receiving a non-compatible or un-healthy organ. Today, Lance continues to wait for his heart at the hospital, while staying in shape and inspiring other patients and friends.
Right now, Lance lives in a hospital room until a donor heart becomes available. Everyday, he speed walks three miles through the hospital hallways with an on-duty nurse who is also required to carry a 17lb. back-up device and batteries. To pass the time, Lance reads, studies Spanish, follows sports, watches the news, visits patients and lifts weights. He even stopped by the waiting room while our Dad was in surgery for transplant on June 26th.
"I am currently in the hospital awaiting a heart transplant. I stay steadfast and strong, waiting to start my new life and to spread the word about the new technological advances to help heart patients. My journey has been long, but fruitful. I've been able to inspire others, to think and dream about what they can do, not what they can't. The TAH has allowed me to have a platform to realize and encourage everyone to live life to the fullest."
We hope Lance gets his heart before his 50th birthday at the end of this year. With all the publicity and awareness he has helped provide for the TAH, Lance deserves more than anyone to retire his machine and move on with his second chance at life. He looks forward to playing basketball, swimming and traveling once he gets to transplant.
Read about and watch Lance's feature by CBS News here.
Meet Steve Williams
“Life leading up to heart transplant and heart transplant themselves can sap a lot of your strength. It will take time and effort to regain strength”
Steve Williams, 55, is a Total Artificial Heart (TAH) and Heart Transplant survivor and also our family’s Angel. I first met Steve Williams on a Monday, in the ICU after my dad’s TAH implantation surgery (February 2016). When I saw his kind, smiling face at the door, I knew exactly who he was—the man from the article! I couldn't believe it.
Before my dad’s surgery, I feverishly researched everything I could find on the TAH. Thankfully, I found an article from The Verge (a technology, science, art and culture site), which shared Steve’s journey to transplant. At this point, the most helpful parts of this article were the photos showcasing life with a TAH. Steve was photographed walking along the beach, playing with his dog, and relaxing in his backyard. I used these images to create a simple TAH presentation to share with my family, friends and other patients in the ICU. Why? Because no one knows what a TAH is unless you or your loved one needs one.
Steve, a dedicated volunteer at Cedars Sinai, took the time to visit my dad and speak with my family about his experience with TAH. Speaking with someone who went through a similar journey gave us a true sense of hope to look forward towards transplant. Steve was often around watching over my dad. When he got transferred out of the ICU, Steve would visit us in the "step down unit" and also in rehab. (My dad's heart was in very bad shape and requires serious physical therapy even today).
Currently, Steve is fifteen months post-transplant and “doing pretty good”.
Steve’s Bridge-to-Heart-Transplant Timeline:
April 2014 – Received the TAH
May 2014—Suffered a stroke
April 2015 – Received a new heart
“I am still trying to get my old strength back - surfing and tennis. But I walk 2-5 miles a day, went camping/hiking in the mountains (9,000 to 11,000 feet) and golfing again. I still have some problems but I am thankful to be alive!
I volunteer at Cedars and yesterday I went to a deli to buy a patient some food. It felt great to help him as he is from NY and has limited help in LA. He was frustrated about his food situation. I also spoke to another patient who did not have a TAH or LVAD. He was amazed with his new heart and could feel the difference (strength of the beating). This has been a pretty consistent feeling of patients going from their bad heart to a new heart. I have spoken to other TAH patients that post-transplant, they did not feel a significant change. I bring this up because the TAH works as behaving like a “good heart”. Thus the TAH helps people get more heart health function - heart rate, kidney and liver health.
Life leading up to heart transplant and heart transplant themselves can sap a lot of your strength. It will take time and effort to regain strength.”
My dad is scheduled to leave the hospital today, 12 days after surgery. We are forever thankful for the support from the staff at Cedars Sinai and also from our friend Steve. My family will always have him in our hearts and hope he continues to do well with his heart transplant.
Read Steve’s journey to heart transplant here.
We Have A Heart!
UPDATE: Surgery went well and my dad is currently recovering in the ICU. We are relieved to get through the first major obstacles of heart transplant.
My Dad is truly lucky. In fact, our entire family is. He is currently in the operating room waiting for the hospital to approve the organ for his heart transplant. We will be in the waiting room for at least 5 hours once the heart is approved. Here are three possible scenarios:
Scenario 1. Dad goes into the O.R. and the heart can get refused by the surgeon. Dad would
Scenario 2. Dad is fully prepped for surgery and the heart is refused by the surgeon
Scenario 3. Dad goes under and the heart is approved by the surgeon and the surgery proceeds
We were scheduled for surgery at 11:30AM. It is currently 2:00PM. At this point, Scenario 1 is invalid because the nurse practitioner has advised my dad is already under anesthesia and we are still waiting for the heart to be approved. We can only hope for the best and not be disappointed if the organ is not right for my Dad.
Thank you to the donor, the family of the donor, the staff at Cedars Sinai, and our loved ones watching from above.
*I took this photo at 5:45AM today after spending the night in my Dad's hospital room. We had received a call from the hospital on Saturday evening around 7:00PM. After rushing to the hospital, we anticipated surgery that night but later learned the procedure would most likely happen the following morning at 11:30AM.
Happy Father's Day
Happiest Father's Day to all the wonderful dads. I am especially thankful to spend today with my loving dad and family. He has gone through a lot in the past year and continues to work hard to gain his strength back. Thank you for being here with us. We do not take it for granted.
Love you Dad!
RE-LISTED! And Getting Used to the “New Normal”
On Friday, April 29th, my dad got re-listed on the transplant list to Status 1B. Status 1B means the patient is dependent on medication or a mechanical-assist device. Above Status 1B is Status 1A which is an urgent need for transplant. In my opinion, being dependent on a TAH certainly qualifies for Status 1A but I don’t get to make the rules. Below Status 1B is Status 2, which means a patient is stable on oral medication and able to wait at home. Then there is Status 7 which means the patient is inactive due to a change in condition. Between my dad’s TAH implantation and Friday, April 29th, my dad was a Status 7 due to his weak condition and failed test results.
Receiving the re-listing confirmation at clinic from our MCS coordinator was the happiest I had seen my dad and family in a long time. Also by luck, we got a chance to meet Lance White, another TAH patient of 2 years during our clinic appointment. Lance is special because my sisters and I got a chance to speak with him before my dad’s TAH implantation surgery back in January. This was facilitated by our thoughtful MCS coordinator. Lance provided my family with optimism, hope and assurance that everything could turn out ok-- and it did.
Since hearing the news of getting re-listed, my dad has found a new motivation and goal to work harder and gather his strength for his future heart transplant.
On Mother’s Day, I stayed home with my dad so my sisters, my husband and Mom could enjoy a nice brunch away from the house. During this time, my dad initiated the desire to walk outside while carrying the 17 lb. Freedom Driver. Before this, I was the ‘bad cop’ who always pushed him with physical therapy and occupational therapy. His motivation and desire to get stronger moved me so much I cried.
Today, we go on as if living with the TAH is the “new normal”. We are still adjusting to the lifestyle which consists of helping my dad with simple things like getting up from bed, using the restroom and putting on clothes. In the back of everyone's mind, I know each family member looks forward to the day we get a call that a matching organ is available. However, there’s no telling when this day will come. So until then, it’s best we live life as if the TAH is the "new normal". Anticipating a heart transplant will only make the days, weeks and months longer.
The Recovery
After heart surgery, the patient’s chest is left open for a few days. This grants rapid access if complications arise including internal bleeding and also allows the swelling to go down. Some patients go into close chest surgery and come out with the chest still open due to swelling issues. The experience is different for everyone. Also note the patient is intubated to assist with breathing. A flexible plastic tube is placed down your trachea, or windpipe and you are unable to speak or eat.
My dad got chest closure surgery two days later. We learned the majority of heart transplant/TAH patients have issues with their gallbladder. As a precaution, the doctors recommended we remove the gallbladder in the middle of surgery. I signed the consent form in the OR lobby. My sister and I youtubed to procedure to better understand what was going to happen in the OR. Over the next few days, many tests were conducted to monitor his brain activity, liver function, blood levels and more. By day four, Dad was able to follow commands. He was still intubated due to mucus build up in his lungs. I could only imaging how uncomfortable he was at this point.
Almost one week after closing his chest and working on his recovery, we had to go back into open chest surgery due to internal bleeding. They removed one liter of clotted blood. This was an emotional time for us after working so hard to get him better. I cried.
Two days later, Dad got to close his chest again. Two days later, we got to extubate Dad. It has been a full two weeks since we were admitted at the hospital.
Dad was able to walk with the assistance of three other nurses and myself the day after Valentine's Day. This was a huge accomplishment. We were excited and hopeful.
It Was Like Winning The Lotto
My dad had been suffering from Congestive Heart Failure (CHF) and in desperate need of a heart transplant since 2012. The symptoms became extremely severe last September 2015, when he lost the ability to walk on his own. After months of medication including a home care peripherally inserted central catheter (picc-line) of Milrinone IV that fed directly to his heart (requires 24 hour care), and multiple visits to the ER due to shortness of breath and fluid build-up in his lungs, my dad reached a point where medicine was not enough. After months of alternative treatment, we knew it would be like winning the lotto if he got approved for a heart transplantation.
Late January 2016, my father was hospitalized due to his Implantable Cardioverter Defibrillator (ICD) going off for the first time since the implantation 4 years ago, due to arrhythmias (irregular heart beats) in his heart. We were lucky enough to get admitted to Cedars Sinai after waiting over two days for a hospital bed to open up in the Intensive Care Unit. *Currently, there are only three heart transplantation centers in Southern California: Cedars Sinai, UCLA and USC.
Less than a few hours after getting admitted, my dad was required for emergency surgery in the catheter lab to receive Extracorporeal Membrane Oxygenation (ECMO) treatment. This bypass machine basically does the job of your heart and lungs by oxygenating your blood back into your body. At this point, you are on advanced life support and cannot be on this treatment for long as it affects other vital organs.
My family was in shock and terrified of the outcome. I signed the consent form so the surgeon could attempt to save his life – which he did. I hate to admit it but minutes before, we had been arguing in the hospital café about future caregiver help. But now, we didn't know if it would be required.
Thankfully the procedure was a success. Our next step was to wait for the staff of Cardiology to present my father’s case and decide if he was eligible for a heart transplant.
There are three requirements to be considered for a heart transplant:
1. Medical assessment
2. No other medical issues
3. Emotional and social support of loved ones
We were thrilled to learn he was approved. Two days later, he was scheduled for surgery. If a donor heart became available, he would receive a heart transplant. Instead, he received a TAH. He was in surgery for 5 hours and we were told he had a 50-60% chance of survival. The nurse for the operating room will take down a point person’s phone number and call you when surgery starts, every hour after that and once surgery is completed. Below was our timeline:
11:20 - Surgery started
12:58 - Surgery in progress
3:00 - Heart is in
4:00 - Surgery complete
***Note: the Operating Room can be quite busy and your scheduled surgery may or may not happen the time or day it was scheduled. You must be patient and trust that your doctors are making the best decisions for your loved one and other patients that need help.
THE RECOVERY Blog coming soon…
Currently
My dad will be 63 this year. Our goal is to see him walk my two sisters (24 and 33) down the aisle and live a fulfiling and happy life into his 80’s.
It has been over two months since my father received a Total Artificial Heart transplantation. Today it has been almost two weeks since discharge and we are currently not on the transplant list. This is considered Status 7 when you are temporarily inactive due to weakness and cannot undergo transplant surgery. He needs to prove his strength to the staff of Cardiologists in order to get presented again. When he does get back on the list, he will be bumped down to a Status 1B because he is not medically at high risk to be on the Status 1A list – unless other complications occur.
I do not like the cards we have been dealt, but we are playing to win.
Welcome
Welcome to Coping Hearts’ website and blog. My goal is provide you and your family the support, guidance and tools to make your experience a little easier by sharing my family’s journey receiving a Total Artificial Heart (TAH). During our extreme time of need, I would have loved the guidance from another person’s experience so I hope this helps you. To provide context 2,000-2,300 heart transplants are performed in the United States annually. In 2015, there were 122 heart transplants performed at Cedars Sinai in Los Angeles alone, and only 17 were Total Artificial Heart procedures. As of February 2016, 9 Total Artificial Heart procedures were completed at Cedars Sinai. Like it or not, we now are part of a unique club and have each other to support. This is for you, the patient, families of the patient and close friends.